Gum disease (Periodontitis)
Have you noticed severe swelling or bleeding every time you brush your teeth? Periodontitis, or gum disease, is more common than you think, but that doesn’t mean you should live with the pain and discomfort.

Treatment
2+ hours

Price
From £600

Team Experience
40+ years
Recovery Time
1+ day

Google Rating
★★★★★ (4.9)

At Wimpole Street Dental Clinic, we can provide periodontitis treatment as soon as we diagnose the disease. We’ll then use a structured recall system to help you prioritise regular dental check-ups and oral health appointments to prevent gum disease in the future.
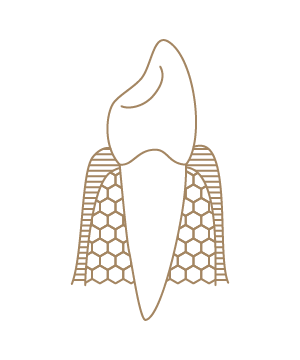
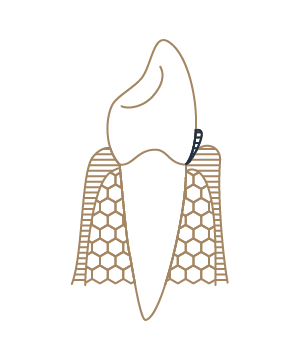
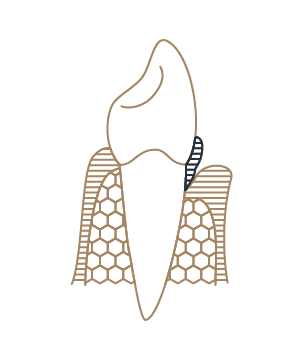
Periodontitis or gum disease presents with symptoms including swelling and bleeding gums. It is a progressive gum health condition that, if left untreated, can lead to bone loss in the mouth, tooth loss and even allow bacteria to enter the bloodstream, causing further health complications such as Diabetes, an increased risk for strokes and heart attacks, and it can impact pregnancy.
Who is suitable for the treatment of periodontitis?
If you are experiencing pain or discomfort regularly from swollen or bleeding gums while you floss or brush your teeth, then please contact us to book an appointment with your dentist or dental hygienist for periodontal treatment. We can diagnose if you have periodontitis gum disease and create your care plan.
Periodontitis is treatable, so give yourself and your dentist the best chance of success by booking an appointment as soon as you experience such symptoms regularly, especially in the early stages of the condition.
Be aware that if you are a smoker, symptoms that would expose a gum disease (e.g. gum problems, bad breath) could be masked. As smokers have a higher risk of developing gum disease, please visit your dentist and hygienist regularly.
What is the cost of periodontitis treatment?
Cost expectations for periodontal disease treatment can be difficult to disclose until your consultation because the price varies from one patient to another. However, the following periodontal disease treatment costs should provide a sense of what to expect for your total fees. Please note that these numbers are ranges; your dental specialist will provide a definite price during your own consultation.
Meet your award-winning Gum Disease dentist and team…
- We have over 75+ years of combined dentistry experience across our specialist team.
- 10,000+ treatments performed and counting.
- We are leaders in the dental industry – we regularly teach, lecture and publish our research work internationally.
Our Expertise
We are proud to offer a full suite of options in the dentistry field of periodontics for you to consider, depending on the severity of your condition as presented.
From your periodontitis diagnosis and review to dental hygiene treatment and cleansing to dental surgery if required.
Our treatment approach for periodontitis includes an emphasis on long-term care with regular dental and dental hygienist appointments with us, so we use a structured recall system to ensure that you never miss a check-up.
The preservation of your oral health with beautiful teeth and healthy gums is the guiding principle of our work.
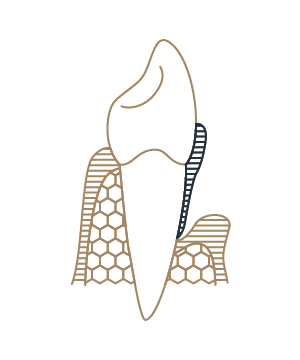
The stages of periodontal disease

HELEN LI
Wimpole Street Dental has the highest most ethical standard of work, personable approach, clear and safe procedures, top notch excellence and reliability in treatment provided with utmost professionalism from crème de la crème world class specialists all under one roof.
What happens during the treatment of periodontitis?
At your appointment, we provide an immediate diagnosis after assessing your current oral health and discussing your current regular dental hygiene. We may ask if you’ve ever suffered from gum disease before to better understand your oral health history.
Your periodontist (a dentist who has extensive experience and expertise in performing periodontal treatment) or hygienist will conduct a careful, meticulous treatment and professional cleaning to remove plaque and tartar from your gum pockets and gum line.
We will schedule a re-evaluation of your gums four to six weeks after today’s treatment appointment to ensure no further inflammation occurs.
If there are still some pockets left, an open debridement will become necessary. The gums are slightly lifted to see the surface of the root, which is then cleaned meticulously.
Your long-term care plan will begin which comprises a commitment to attend regular check-up appointments with both your dentist and your dental hygienist to keep the gum inflammation you have experienced at bay.
Take your first step with Wimpole Street Dental Clinic
Discover the path to a brighter smile with Wimpole Street Dental Clinic! Our team of skilled professionals utilises advanced technology to provide personalised dental care in a comfortable setting.












New page design
Written by: Prof Dr Christian Mehl
Medically reviewed by: Dr Raul Costa
Author biography added
Written by: Prof Dr Christian Mehl
Medically reviewed by: Dr Raul Costa
Original content created
Written by: Prof Dr Christian Mehl
Medically reviewed by: Dr Raul Costa
Wimpole St Dental Clinic has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Kwon T, Lamster IB, Levin L. Current Concepts in the Management of Periodontitis. Int Dent J. 2021 Dec;71(6):462-476. doi: 10.1111/idj.12630. Epub 2021 Feb 19. PMID: 34839889; PMCID: PMC9275292.
- Dannewitz B, Holtfreter B, Eickholz P. Parodontitis – Therapie einer Volkskrankheit [Periodontitis-therapy of a widespread disease]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2021 Aug;64(8):931-940. German. doi: 10.1007/s00103-021-03373-2. Epub 2021 Jul 8. PMID: 34236451; PMCID: PMC8264996.
- Slots J. Periodontitis: facts, fallacies and the future. Periodontol 2000. 2017 Oct;75(1):7-23. doi: 10.1111/prd.12221. PMID: 28758294.
- Bartold PM. Lifestyle and periodontitis: The emergence of personalized periodontics. Periodontol 2000. 2018 Oct;78(1):7-11. doi: 10.1111/prd.12237. PMID: 30198129.






